1. Endometriosis: Basics, Statistics, and Emotional Impact
Endometriosis, a complex medical condition affecting millions of women globally, demands attention and understanding. In this comprehensive guide, we delve into the fundamental aspects of endometriosis, offering insights into its definitions, statistics, symptoms, emotional impact, and factors influencing its occurrence.
Key Points
Table of contents
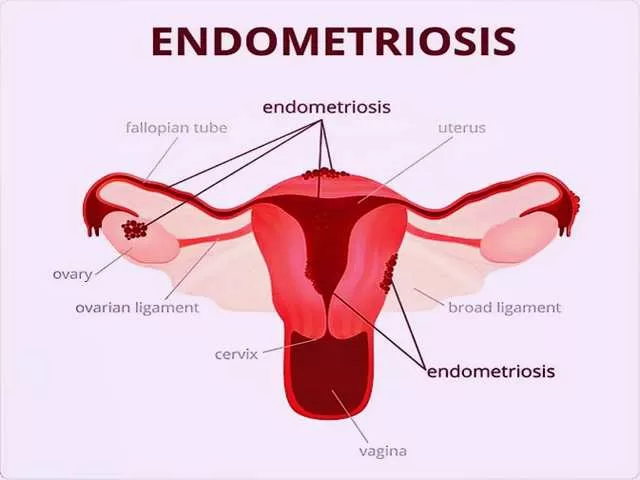
1.1. What is Endometriosis?
Endometriosis is a condition where the lining of the uterus grows outside of the uterus, manifesting in areas referred to as lesions, growths, implants, or nodules.
1.2. Statistics
In North America alone, approximately 5.5 million women grapple with endometriosis. A staggering 30-40 percent of these women face infertility issues, positioning endometriosis as one of the top three causes for female infertility.
1.3. Where is it Found?
Endometriosis manifests in various locations within the body:
- On the ovaries
- On the bladder
- Behind the uterus
- On the uterus tissues
1.4. Symptoms
Recognizing the symptoms is crucial for early diagnosis and management:
- Painful menstrual cramps worsening over time
- Pain during or after sex
- Infertility
- Intestinal pain
- Chronic pain in the lower back and pelvis
- Fatigue
- Painful urination during menstrual periods
- Painful bowel movements
- Heavy menstrual periods
- Spotting or bleeding between periods
1.5. Emotional Symptoms
Endometriosis extends beyond physical implications, impacting women emotionally. Seeking support from psychologists or counselors is vital to cope with emotions such as confusion, disbelief, and frustration.
1.6. Who is Affected?
Understanding the demographic affected by endometriosis:
- Symptoms persist for two to five years before diagnosis
- Onset of monthly periods has begun
- Average age is around 27 years
1.7. What Raises the Risk?
Several factors elevate the risk of developing endometriosis:
- Early onset of menstruation
- Periods lasting more than seven days
- Heavy menstrual flow
- Family history of endometriosis
- Short menstrual cycles
1.8. What Reduces the Risk
Studies suggest potential risk reduction by:
- Avoiding caffeine and alcohol
- Regular exercise
1.9. Cancer Risk
A mild risk of ovarian cancer is associated with endometriosis. Theories propose that endometriosis nodules may transform into cancer or that genetic and environmental factors related to endometriosis could contribute to ovarian cancer.
Understanding endometriosis is paramount in fostering awareness, facilitating early diagnosis, and providing the necessary support for those affected. By exploring the intricacies of this condition, we aim to contribute to a broader understanding of endometriosis and its multifaceted impact on women’s health.
2. Diagnosing and Treating Endometriosis
In this segment, we delve into the pivotal aspects of diagnosing endometriosis and shed light on the various treatments available for individuals grappling with this complex condition.
2.1. Why Diagnosing is Important
Endometriosis poses challenges for conception, making early diagnosis crucial. Uncover the significance of detecting endometriosis, as timely interventions can alleviate pain and enhance fertility, topics we’ll explore further in this guide.
2.2. How Endometriosis is Diagnosed
Several diagnostic tests aid in identifying endometriosis:
- Ultrasound
- MRI
- Laparoscopy (discussed later in this guide)
2.3. Tests
A closer look at diagnostic tests:
- Biopsy (via laparoscopy)
- Laparotomy
Detailed discussions on these tests follow in subsequent sections.
2.4. Healthcare Professionals
A collaborative effort of healthcare professionals can significantly impact endometriosis management. The team may include gynecologists, surgeons, nutritionists, dieticians, psychologists, counselors, and pain specialists.
3. Treatments
3.1. Pain Medication
Over-the-counter medications that effectively manage endometriosis pain:
- Ibuprofen
- Naproxen
- Tylenol
- Midol
3.2. Hormone Treatment
Insights into hormone medications recommended by doctors, particularly beneficial for women with smaller growths and milder pain. Considerations regarding fertility are highlighted.
3.3. Nutritional Therapy
Understanding the role of nutritional therapy in managing endometriosis symptoms. Explore how a healthier diet can enhance treatment tolerance, boost energy levels, and improve mental clarity. Nutritionists play a crucial role in developing personalized plans.
3.4. Alternative Therapy
An exploration of alternative therapies embraced by some women with endometriosis:
- Homeopathy
- Osteopathy
- Herbal treatments
- Yoga
- Pilates
Empowering individuals with diverse approaches, this guide aims to provide comprehensive insights into diagnosing endometriosis and navigating the array of available treatments. By unraveling the complexities of this condition, we aspire to contribute to a broader understanding and facilitate informed decisions for those affected by endometriosis.
4. Importance of Support and Valuable Resources
In this segment, we unravel the significance of support networks and provide essential resources for individuals navigating the complexities of endometriosis. Additionally, we delve into the latest research and explore theories surrounding the potential causes of this condition.
4.1. Support Groups
Endometriosis often brings forth a myriad of emotions. Joining a support group, whether in-person or online, provides an invaluable opportunity to connect with other women facing similar challenges. Discover the strength that communal understanding and shared experiences can offer.
4.2. Research
Ongoing research aims to unveil new medical treatments for endometriosis-related pain. Stay informed about clinical studies and trials by calling 1-800-411-1222 or visiting the NIH Clinical Trials Web site at https://clinicaltrials.gov. Participating in research contributes to advancing our understanding and treatment options.
4.3. Resources
Explore a range of endometriosis resources:
- National Women’s Health Information Center: 1-800-994-9662
- Endometriosis Association: 414-355-2200, www.endometriosisassn.org
- The American College of Obstetricians and Gynecologists: www.acog.org
- Endometriosis Research Center: 800-239-7280, www.endocenter.org
5. CAUSES
While definitive causes for endometriosis remain elusive, the following set of tips explores various theories that attempt to shed light on potential origins.
5.1. Blockage
The daily shedding of blood and tissue into the body can lead to inflammation and pain over time. This tissue’s growth may cover the ovaries and fallopian tubes, impacting fertility.
5.2. Faulty Immune System
Some scientists propose that women with endometriosis may exhibit certain immunologic defects or dysfunctions. However, the nature of this relationship—whether it’s a cause or effect—is yet to be fully understood.
5.3. Metaplasia
Metaplasia involves the transformation of one normal tissue type into another. Researchers suggest that endometrial tissue may, in some instances, replace other types of tissues outside the uterus.
5.4. Retrograde Menstruation
This theory posits that menstrual tissue flows backward through the fallopian tubes, leaving deposits on pelvic organs where it can seed and grow. However, researchers note that the majority of women experience retrograde flow without developing endometriosis.
5.5. Genetics
Studies indicate a higher likelihood of endometriosis in first-degree relatives of affected women, hinting at a genetic component in this complex condition.
5.6. Lymphatic Distribution
Researchers theorize that fragments from endometriosis may travel through the blood or lymphatic system to other parts of the body, potentially explaining its presence in various locations.
5.7. Environmental
Controversial studies suggest environmental factors could contribute to endometriosis. Toxins, in particular, may impact reproductive hormones and the immune system.
By delving into these theories, we aim to foster a better understanding of endometriosis, empowering individuals to navigate their journey with the support and resources needed for comprehensive care.
6 Endometriosis: Hormone Treatments
In this comprehensive guide, we unravel the intricacies of hormone treatments available to women grappling with endometriosis. From established methods like birth control pills to cutting-edge options, we delve into how these treatments alleviate symptoms, providing relief and empowerment.
6.1. Birth Control Pills
Birth control pills emerge as a frontline defense against the pain of endometriosis. By preventing the monthly build-up and breaking down any potential growths, these pills offer significant relief. Their hormonal balance proves instrumental in managing the condition’s impact on the menstrual cycle.
6.2. Progestins
Designed specifically for women unable to take estrogen, progestins function similarly to birth control pills. They not only alleviate pain but also contribute to lighter and shorter menstrual periods, offering a tailored solution for those with specific hormonal sensitivities.
6.3. GnRH Agonists
Gonadotropin Releasing Hormone Agonists (GnRH Agonists) play a pivotal role in slowing down the growth of endometriosis, effectively relieving associated symptoms. By reducing the levels of estrogen in the body and halting the monthly cycle, these agonists bring significant respite to individuals dealing with the condition’s impact.
6.4. Danazol
Although less commonly used today, Danazol, a weak male hormone, operates in a manner akin to GnRH Agonists. It diminishes the growth of endometriosis but may trigger side effects like weight gain, oily skin, breast size reduction, fatigue, and hot flashes. While its application has declined, it remains part of the historical landscape of endometriosis treatment.
6.5. Mirena
Mirena, a Progestin Intrauterine Device (IUD), stands out as a distinctive contraceptive method that also addresses endometriosis. By preventing ovulation and altering the uterine lining to deter implantation, Mirena offers a unique blend of birth control and therapeutic benefits for women dealing with this condition.
6.6. Aromatase Inhibitors
Representing a newer frontier in endometriosis treatment, aromatase inhibitors have shown promise in studies. Despite the limited number of patients involved, research indicates their effectiveness. However, it’s crucial to note that the exploration of endometriosis treatment with aromatase inhibitors is still in its early stages, necessitating ongoing research and clinical development.
As we navigate through the spectrum of hormone treatments, it’s evident that medical advancements continue to expand the toolkit for managing endometriosis. Each option plays a distinct role, contributing to the tailored care and holistic well-being of individuals facing this challenging condition.
7. Surgical Solutions for Endometriosis
In the ongoing exploration of endometriosis, this segment delves into various surgical interventions aimed at both diagnosing and treating this complex condition. From minimally invasive procedures to more extensive surgeries, each approach serves a unique purpose in addressing the challenges posed by endometriosis.
7.1. Laparoscopy
Laparoscopy stands out as a pivotal surgical procedure for diagnosing and treating endometriosis. With a small incision in the abdomen, doctors insert a thin tube equipped with a light to visualize and remove endometrial growths and scar tissue causing pain. This minimally invasive technique facilitates accurate diagnosis and targeted treatment.
7.2. Laparotomy
For cases requiring a more extensive approach, laparotomy involves a larger abdominal incision. This allows doctors to reach inside and surgically remove endometrial growths in the pelvis or abdomen. While effective, the recovery period for laparotomy can extend up to two months, emphasizing the need for careful consideration of the procedure’s impact.
7.3. Hysterectomy
Hysterectomy emerges as a permanent surgical solution, recommended for women no longer seeking pregnancy. In this procedure, the uterus is removed, and in some cases, the ovaries and fallopian tubes may also be extracted. Hysterectomy offers a definitive resolution for endometriosis-related challenges, but the irreversible nature of the surgery necessitates thoughtful decision-making.
7.4. Presacral Neurectomy
A specialized intervention, presacral neurectomy, involves the surgical cutting of nerve fibers connected to the uterus. While highly effective in alleviating symptoms, this procedure may present long-term side effects such as constipation and urinary urgency. Careful consideration of the potential consequences is essential when contemplating presacral neurectomy.
Navigating the landscape of surgical options for endometriosis underscores the importance of tailored approaches to individual cases. The choice between laparoscopy, laparotomy, hysterectomy, or presacral neurectomy depends on factors such as the severity of symptoms, reproductive goals, and overall health. Consulting with a healthcare professional becomes crucial in making informed decisions aligned with the specific needs and circumstances of each individual.
As we uncover the array of surgical solutions available, it becomes evident that a multidisciplinary approach, involving open communication between patients and healthcare providers, is paramount. By demystifying these surgical interventions, we empower women to actively participate in decisions regarding their health, fostering a collaborative journey toward managing and overcoming endometriosis.
Endometriosis: Clearing Misconceptions and Answering FAQs
Progressing from hydrosalpinx, hematosalpinx involves the blockage of blood in the fallopian tubes. Gain insights into this chronic condition, drawing distinctions from tubal pregnancies.
Unpack the term “hydrosalpinx,” understanding it as a collection of fluid in a blocked fallopian tube. This section delves into the implications and connections to endometriosis.
Discover the significance of CA-125, a membrane antigen whose elevated levels in women with endometriosis hint at potential diagnostic applications. Explore the evolving landscape of diagnostic tools.
Some women may harbor endometriosis without evident symptoms. This section discusses the possibility of asymptomatic cases, emphasizing the importance of awareness and timely diagnosis.
Understanding pelvic adhesions involves exploring the scarring of the peritoneum, often linked to the irritation caused by menstrual blood. This insight sheds light on an aspect of endometriosis-related complications.
Unveil the mystery behind “chocolate cysts” or endometriomas, exploring their formation as endometriosis infiltrates ovarian tissue and gives rise to fluid-filled cysts.
Research indicates that using tampons and douching likely does not increase the risk of endometriosis. This section delves into the relationship between menstrual hygiene practices and the condition.
Debates surround the impact of tubal ligation on endometriosis. This guide explores existing perspectives, offering insights into the potential protective effects or lack thereof.
Endometriosis is not cancer, though its cysts may mimic tumors. Understanding the distinction is vital for accurate information dissemination and addressing concerns about the condition’s nature.
Fertility concerns affect 30-40% of women with endometriosis. Open communication with healthcare professionals can lead to personalized treatment plans, addressing worries and promoting informed decisions.
Researchers propose hereditary links to endometriosis, with first-degree relatives showing increased susceptibility. Delving into these theories sheds light on the potential genetic factors contributing to the condition.
Endometriosis is not contagious and cannot be transmitted between individuals. Research dismisses the notion of infectious origins, highlighting the need for accurate information regarding the condition’s nature.
Endometriosis typically persists throughout a person’s life, but symptoms may lessen after menopause as the growths gradually diminish. Understanding the trajectory of the condition offers valuable insights into long-term management.
While there’s no cure for endometriosis, effective management strategies exist. This guide explores various available treatments to help individuals alleviate symptoms and lead fulfilling lives.
As we unravel the intricacies of endometriosis, this guide aims to empower individuals with knowledge, fostering informed discussions with healthcare professionals and promoting a proactive approach to managing this multifaceted condition.